- About Us
- Associated Clinics
- Treatment
- Line & Wrinkle Freezing
- Wrinkle Fillers
- Facial Implants
- Skin Peels
- Active skin care
- Acne treatment
- Mole, Skin and Wart Removal
- Pigmented Lesions
- Leg and Facial Veins
- Microdermabrasion
- Stretch mark removal
- Thread vein removal
- Hair removal
- Tattoo removal
- Mesotherapy
- Laser Skin Therapy
- Laser Fungal Nail Infection
- Skin Regeneration
- Sublative Rejuvenation
- Skin Tightening
- Excessive Sweating
- Polycystic OS
- Aqualyx
- PRP Platelet-Rich Plasma
- Syringoma
- Contact
What is fungal infections?
Fungal infections of the skin are also known as 'mycoses'. They are common and generally mild. However, in very sick or otherwise immune suppressed people, fungi can sometimes cause serious disease.
Characteristics of fungi
Fungi are parasites or saprophytes i.e. they live off living or dead organic matter.
Mycologists identify and classify fungi according to their appearance by microscopy and in culture, and by the method of reproduction, which may be sexual or asexual.
Growing fungi have branched filaments called hyphae, which make up the mycelium (like branches are part of a tree). Some fungi are compartmented by cross-walls (called septae).
Arthrospores are made up of fragments of the hyphae, breaking off at the septae. Asexual spores (conidia) form on conidiophores. The sexual reproductive phase of many fungi is unknown; these are 'fungi imperfecta' and include those which infect humans.
Yeasts form a subtype of fungus characterised by clusters of round or oval cells. These bud out similar cells from their surface to divide and propagate. In some circumstances they form a chain of cells called a pseudomycelium.
Superficial fungal infections
These affect the outer layers of the skin, the nails and hair. The main groups of fungi causing superficial fungal infections are:
- Dermatophytes (tinea)
- Yeasts i.e. candida, malassezia, piedra
- Moulds.
Subcutaneous fungal infections
These involve the deeper layers of the skin (the dermis, subcutaneous tissue and even bone). The causative organisms normally live in the soil living on rotting vegetation. They can get pricked into the skin as a result of an injury but usually stay localised at the site of implantation. Deeper skin infections include:
- Mycetoma
- Chromoblastomycosis
Systemic fungal infections
Systemic mycoses may result from breathing in the spores of fungi, which normally live in the soil or rotting vegetation or as opportunistic disease in immune compromised individuals.
Inhaled fungal infection
Although uncommon, some may infect healthy individuals. The result is most often a mild infection and long lasting resistance to further attack, but occasionally these infections are more serious and chronic (especially in the immune suppressed). The organisms causing systemic fungal infections include:
- Histoplasmosis
- Coccidioidomycosis (North and South America).
Opportunistic infection
Other systemic mycoses only infect those who are already sick or immune suppressed i.e. they are 'opportunists'. Repeated infection may occur. Risks for systemic mycoses include:
- Serious illness and debility
- Cancer or leukaemia
- Diabetes mellitus
- Transplant
- Massive doses of antibiotics
- Parenteral nutrition
- Drug addiction
- Infection with human immunodeficiency virus (HIV)
Opportunistic fungal infections include:
- Aspergillosis (found everywhere)
- Mucormycosis
- Cryptococcosis (where there are pigeon droppings)
- Trichosporon beigelii
- Pseudallescheria boydii.
Characteristics of fungi
Fungi are parasites or saprophytes i.e. they live off living or dead organic matter.
Mycologists identify and classify fungi according to their appearance by microscopy and in culture, and by the method of reproduction, which may be sexual or asexual.
Growing fungi have branched filaments called hyphae, which make up the mycelium (like branches are part of a tree). Some fungi are compartmented by cross-walls (called septae).
Arthrospores are made up of fragments of the hyphae, breaking off at the septae. Asexual spores (conidia) form on conidiophores. The sexual reproductive phase of many fungi is unknown; these are "fungi imperfecta" and include those which infect humans.
Yeasts form a subtype of fungus characterised by clusters of round or oval cells. These bud out similar cells from their surface to divide and propagate. In some circumstances they form a chain of cells called a pseudomycelium.
Laboratory tests for fungal infection
To establish or confirm the diagnosis of a fungal infection, skin, hair and nail tissue is collected for microscopy and culture (mycology).
Long wavelength ultraviolet radiation (Wood lamp) can help identify some fungal infections of hair (tinea capitis) because the infected hair fluoresces green.
Specimen collection
Specimens for fungal microscopy and culture may be:
- Scrapings of scale, best taken from the leading edge of the rash after the skin has been cleaned with alcohol.
- Skin stripped off with adhesive tape, which is then stuck on a glass slide.
- Hair which has been pulled out from the roots.
- Brushings from an area of scaly scalp.
- Nail clippings, or skin scraped from under a nail.
- Skin biopsy.
- Moist swab from a mucosal surface (inside the mouth or vagina) in a special transport medium.
- A swab should be taken from pustules in case of secondary bacterial infection.
They are transported in a sterile container or a black paper envelope.
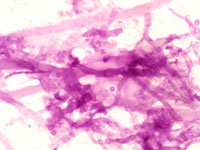
PAS stain of aspergillus seen in a skin biopsy

Potassium hydroxide (KOH) preparation of microsporum canis
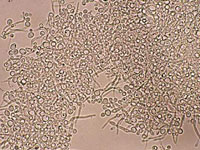
KOH preparation of candida showing pseudohyphae
Direct microscopy
The material is examined by microscopy by one or more of these methods:
- Potassium hydroxide (KOH) preparation, stained with blue or black ink
- Unstained wet-mount
- Stained dried smear
- Histopathology of biopsy with special stains, e.g., periodic acid-Schiff (PAS).
Microscopy can identify a dermatophyte by the presence of:
- Fungal hyphae (branched filaments) making up a mycelium
- Arthrospores (broken-off spores)
- Arthroconidia (specialised external spores)
- Spores inside a hair (endothrix) or outside a hair (ectothrix).
Fungal elements are sometimes difficult to find, especially if the tissue is very inflamed, so a negative result does not rule out fungal infection.
A yeast infection can be identified by the presence of:
- Yeast cells, which may be dividing by budding
- Pseudohyphae (branched filaments similar to those of a dermatophyte) forming a pseudomycelium.
Culture
Culture identifies which organism is responsible for the infection:
- To find out the source of infection e.g. a particular animal
- To select the most suitable treatment.
Growing the fungus in culture may take several weeks, incubated at 25-30oC. The specimen is inoculated into a medium such as Sabouraud's dextrose agar containing cycloheximide and chloramphenicol. The cycloheximide is left out if a mould requires identification.
A negative culture may arise because:
- The condition is not due to fungal infection.
- The specimen was not collected properly.
- Antifungal treatment had been used prior to collection of the specimen.
- There was a delay before the specimen reached the laboratory.
- The laboratory procedures were incorrect.
- The organism grows very slowly.
Culture of yeasts and moulds may be due to harmless colonisation rather than infection. The infection may be secondary to an underlying skin disesase such as psoriasis.
Blood tests
Blood tests are not useful for the diagnosis of superficial fungal infections. But in subcutaneous and systemic infection, several tests may be useful.
- Culture
- Antibodies (histoplasmosis, coccidioidomycosis)
- Antigen (cryptococcosis, aspergillus, candidosis, histoplasmosis)
Treatment of fungal infections
- General measures
- Reducing reinfection
- Topical antifungal medications
- Oral antifungal medications
The trade names of the medications sold in New Zealand are given in parentheses.
General measures
- Correct predisposing factors where possible.
- Keep the affected skin clean and dry. Wash daily. Take care to dry between the toes and in the skin folds; use a hair dryer if necessary. Use your own towel.
- Carefully clean the shower or bath using bleach.
- Hot wash socks, towels, bathmats at a temperature of at least 60C.
- Regularly wash floors where you walk bare foot.
-
Antiseptics
- Dequalinium chloride lozenges for oral candidiasis (Dequacaine®, Dequadin®)
- Di-iodohydroxyquinoline for vulvovaginal candidiasis (Floraquin® vaginal tablets).
To reduce reinfection
Fungal spores can survive long periods. To reduce the chance of reinfection:
- Do not share towels, sheets or personal clothing.
- Avoid walking bare foot where others may tread - wear jandals, sandals or aquasocks at the public pools and sports changing rooms.
- Avoid long periods wearing the same clothing, or wearing occlusive clothing such as wet weather gear and nylon pantyhose.
- Wear open-toed sandals when possible. Avoid long periods in occlusive footwear such as gum boots or tramping boots.
- Use antifungal foot powder e.g. ciclopirox (Batrafen®), econazole (Pevaryl®), miconazole (Daktarin®, Fungo®), tolciclate (Tolmicen®), tolnaftate (Tinaderm®), undecylenic acid (Mycota®). Sprinkle it in your shoes.
- In the case of zoophilic fungal infections, infected animals should be identified and treated.
